This is one of a two-part series following the Fort Lauderdale shooting that occurred on January 6, 2017.
The recent active shooter incident at Fort Lauderdale–Hollywood International Airport on January 6, 2017 that took the lives of five people raised, once again, issues over gun laws, security and civilian safety. While mass shootings in Canada have been more of an intermittent punctuation in long stretches of relative peace, Canadians are not immune to aggressive events of this nature, which tend to draw the attention of soft targets in public spaces with the intent of inciting fear and chaos. Motivations aside, a more common scenario is evolving which places civilians at the scene in a potential role as first care providers.
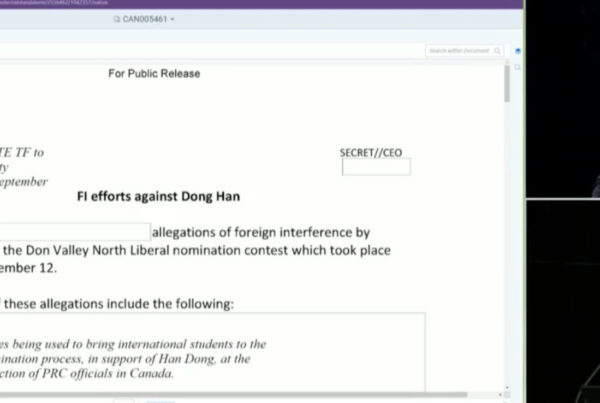
A recently released FBI study on active shooter incidents in the US studied 160 incidents between 2000 and 2013. Of the findings, the study notes that active shooter incidents are becoming more frequent – from 6.4 incidents per year during the first seven years, to 16.4 in the last seven years. The largest percentage of incidents took place in commercial environments (45.6 per cent), followed by 24.3 per cent at academic institutions.[1]

Source: Federal Bureau of Investigation, 2014[2]
Hemorrhage is responsible for 30 to 40 per cent of trauma mortality, of which 33 to 56 per cent occur before the injured make it to a trauma centre.[3] The urgent need to control external hemorrhage on site led to the Hartford Consensus III,[4] which focuses on empowering the public to provide emergency care. Traditionally thought of as bystanders – a person who is present at an event or incident but does not take part – these immediate responders should no longer be considered passive observers. “During intentional mass-casualty events, those present at the point of wounding have often proven invaluable in responding to the initial hemorrhage control needs of the wounded,”[5] writes Dr. Lenworth Jacobs, American College of Surgeons (ACS) Regent and Chairman of the Hartford Consensus. Immediate responders often perform a critical step in eliminating preventable prehospital deaths by controlling external hemorrhage. The Hartford Consensus recommends that legal protections under jurisdictional Good Samaritan laws be extended to include the provision of bleeding control.[6]
The existing emergency response model relies upon an immediate availability of highly trained medical responders. Unfortunately, there are often delays in response times of professional first-responders accessing victims at the scene, especially in highly complex events where it may not be safe for EMS to enter the hot-zone if the area hasn’t been secured (e.g. the attacks in Norway, the Aurora, CO shooting, the Westgate Mall attack in Nairobi). Despite initiatives in the US to create warm zones where it is safe for EMS to administer care, there remains a time gap from point of injury to medical intervention by professional first responders.[7] This gap can and should be managed by those first on the scene – who are increasingly civilian bystanders.
Transition of cardiopulmonary resuscitation (CPR) from a hospital-based intervention to a public domain standard of care began in the 1970s. Over the last four-and-a-half decades, bystander immediate response has evolved to include the use of automatic external defibrillators and stroke recognition.[8]
Bystanders will always be present and will act effectively to assist the emergency response if given the tools to do so. “The keys to successfully transforming bystanders into effective First Care Providers are a combination of community education and training, first responder integration, and the development of standard operating procedures that address scene security, communication, education, and commitment to a tiered whole of community response paradigm.”[9]
Formally, the First Care Providers (FCP) program is a US non-profit organization based upon guidelines formulated in 2011 that identified the need of civilians to provide pre-hospital care.[10] The impetus for public responders harkens back to a time of greater civilian resilience and a presently increasing frequency of events that are geographically isolated or where timely first responder access is hampered by operational barriers. Civilian immediate responders decrease the time between injury and life-saving medical care. “The evolving threat matrix and escalating complexity of mass violence incidents will overwhelm most professional response agencies and demands initiation of a community based response network. First Care Providers are critical to mitigating this risk.”[11] But transforming bystanders into responders requires more than just being Good Samaritans; a unified commitment is required by national or provincial policy makers, first response agencies, and community leaders to provide training opportunities. Over-reliance on the traditional EMS structure means that communities prepare for emergencies based on an assumption that medical care is readily available. We must evolve past such over-reliance and introduce policies that empower the public to perform life-saving medical interventions when professionals are not present.[12]
Traditional command and control models marginalize bystanders and uninjured persons at the scene. First care providers can serve as critical force-multipliers in the response if first-response agencies are familiar with civilian first care provider capabilities and are prepared to integrate this recognition into their operational plans. Data from around the world demonstrates that training individuals empowers action and improves survival from traumatic emergencies.[13]
Community public safety campaigns should promote “run, hide, fight” training for citizens working or attending institutions vulnerable to terrorism such as schools, government buildings, and religious institutions. In addition to effective training programs, these same vulnerable institutions may want to have first-aid supplies readily available. The use of tourniquets has received much criticism over the years, largely based on secondary injury caused by improper placement and/or incorrect pressure that either doesn’t stop the bleed or is left on for too long leading to ischemia and nerve damage.[14],[15] Tourniquets can be a critical life saver if used correctly. A public access trauma kit such as the new interactive mobile rescue system provides all the resources an untrained bystander would need to save a life while EMS in en route. The system harnesses an advanced medical algorithm through an interactive app that will instruct a medical layperson how to assess and triage the injured, and with the aid of organized and colour coded medical equipment, can provide life-saving care in real time.
The current era of random and unpredictable mass casualty incidents in public spaces requires a more engaged citizenry to fill the time gap between point of trauma and access to professional emergency medical care. Logistical issues inherent in complex emergencies require new considerations in our civil emergency preparedness and response plans. Empowering civilian immediate responders or First Care Providers to enter the trauma chain of survival through interventions such as external hemorrhagic control can save many lives in high threat environments. Amanda Ripley, author of The Unthinkable: Who Survives When Disaster Strikes – and Why, says, “regular people are the most important people at a disaster scene, every time.”